Highlights

We stated earlier that the mental healthcare (MHC) reform in Belgium aims to prevent hospitalisation as much as possible. If hospitalisation is nevertheless unavoidable, the stay should be as short as possible. To succeed in this objective, a number of initiatives were launched, including mobile operations, primary psychological function and intensification of residential care provisions.
Mobile functions
|
The aim of the MHC reform is to bring care as close to patients as possible, and respond to their needs and preferences in the best possible way. To this end, multidisciplinary mobile teams were set up to provide specialised care in the home environment of patients with severe psychiatric disorders. Rapid intervention by the crisis team means that treatment can be started in the home environment, potentially avoiding hospitalisation. |
 |
After several weeks of care from the crisis team (known as the 2A team in the adult mental health networks), aftercare can be taken over by a long-term care team responsible for rehabilitation and recovery (2B team in the adult mental health networks). This is also possible immediately after an admission. This makes it possible to keep the hospitalisation period as short as possible, so that the link with the patient’s home, work and learning environments can be restored more quickly.
| In 2022, 157 FTEs were active in the mobile crisis teams and 106 FTEs in the long-term care teams of the MHCY networks. In the adult mental health networks, there were 539 FTE active in 2A teams and 620 FTE active in 2B teams in 2023. |
The 2018 - 2022 evolution indicates that the number of individuals for both the 2A and 2B adult mobile teams show an upward trend[1].
Evolution followed by 2A-team
|
Evolution followed by 2B-team
|
Psychological care in primary care
In April 2019, a pilot project was launched in which doctors can refer patients with mild and moderately severe mental health problems to a clinical psychologist or clinical remedial education provider for short-term, first-line psychological treatment that is largely reimbursed by the health insurance fund. The objective of this is to provide psychological care early and in individuals’ nearby environments.
The treatment consists of a series of individual discussion sessions. An intake interview with diagnosis is followed by treatment sessions. In addition, if the patient needs more intensive, long-term support, the provider may refer the patient.
Mild and moderately severe mental health problems are defined as mental health problems related to anxiety, depressed mood, alcohol abuse or abuse of sleeping pills and sedatives. For adolescents, these can include behavioural or social problems and addiction to screens (smartphone, tablet, laptop, etc.).
In 2020, an agreement was reached in the IMC Public Health, primarily on strengthening the care offering in front-line healthcare, which provided a recurrent budget of 200 million euros.
The agreement sets out several priority target groups, including children and parents in vulnerable families, young adults and people with existing mental health problems. The goal concerns prevention, early detection and early intervention of mild to moderately severe problems through 2 psychological functions:
- resilience-enhancing function
- treatment function of moderate intensity.

In 2022, we found that almost twice as many services under the convention for primary psychological care are billed for women. People who use this type of assistance come mainly from the active population. Among men, we see a high peak in the 10 to 14 age group.
Number of services billed under the first-line psychological care convention, broken down by gender in 2022
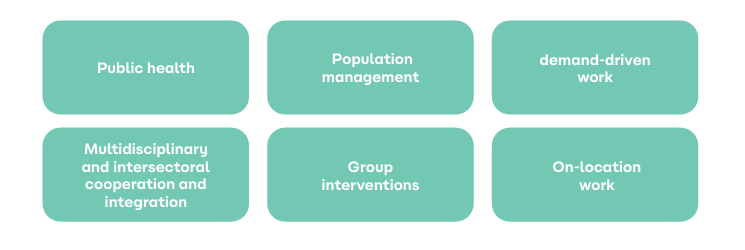
The innovative project is built on a few key pillars to keep the threshold of access to care as low as possible.
A scientific study was recently completed (EPCAP) showing that primary psychological care is effective and efficient: there is an improvement in general functioning, plus there is a reduction in absenteeism, a strengthening of resilience, and a decrease in the waiting time to seek help.
More information EPCAP research report
More information Primary and specialised psychological care in a mental health network - NIHDI (fgov.be)
Residential intensive treatment units HIC and ID
If deemed necessary, more intensive psychiatric care should be offered for more severe mental illness.
To this end, 2 models have been developed:
1. ID model
This involves the creation of a unit for intensified psychiatric care. Here, high-quality, intensified care is realised through the adaptation of care methods on the one hand, and through the adaptation of architecture (low-stimulus rooms, comfort rooms, etc.) or care organisation (smaller living units, etc.) on the other hand.
2. High Intensive Care (HIC) model.
This is a new care organisation model based on the combination of intensified service and increased intensified operations. A ward consists of two smaller adjoining ‘high care units’, supplemented by a separate ‘intensive care unit’. The patient never stays there alone, but is always accompanied by someone from the care staff.
HIC units need to provide better and more humane care for people admitted in crisis. Furthermore, the objective is to reduce aggression and suicidality and further reduce the number of coercive and restrictive measures, such as isolation and fixation.
At least 1 HIC service should be provided in each mental health network within a crisis care pathway. The already existing 9 HIC projects have been expanded to 28 HIC services since 2022.
 |
The ultimate goal of intensifying residential care is to roll out a crisis care pathway throughout Belgium. Each network should review its existing crisis care offerings and then roll out a crisis care pathway according to the stepped care principle. This consists of the collaboration of various players in the network: specifically, HIC services and ID services and the outpatient network including the mobile crisis team and emergency services. Cooperation between these partners is being strengthened. |
More information https://www.psy107.be/index.php/fr/organe-de-concertation/groupe-du-travail-intensification
[1]For the MHCY networks, no figures can be made available at this time.
